Breast surgery
Adnexa surgery
Uterine surgery
Cervical surgery
Vulvar surgery
Other
Hysterectomy

Definitions
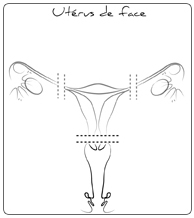
The hysterectomy is the ablation of the uterus. We speak of a complete hysterectomy when the uterus is entirely removed (body and cervix) and of a partial hysterectomy (also called “supracervical”) when the uterine body is removed while leaving the cervix of the uterus. At the time of this operation, it may be required to remove the ovaries with the fallopian tubes.
Surgical techniques
The surgical operation is proposed with either total anesthesia or a regional one (epidural block or spinal anesthesia).
The hysterectomy can be performed in 3 different ways:
Vaginal Hysterectomy
The operation is performed transvaginally that induces no abdominal incision. However, the surgeon may need to practice a laparoscopy to facilitate surgery stage.
Laparoscopic Hysterectomy
The removal of the uterus is done under the control of a camera placed through a single incision on the belly button, and by using trocars just above pubis. At the end of the operation, the uterus can be removed via vagina, or it is cut into small pieces and removed from abdominal cavity via laparoscopic ports. The healing and recovery times are the same than the vaginal hysterectomy.
Hysterectomy via laparotomy
More rarely, the operation is performed by an incision through the abdominal wall, generally horizontal, sometimes vertical, between the pubic bones and the belly button.
The hospital stay is approximately 3 days with a vaginal or a laparoscopic hysterectomy, and 6 days for the abdominal procedure. The work leave is respectively 15 days to 1 month.
Postoperative recoveries
The main clinical manifestations after a hysterectomy are the lack of the menses and the unability to be pregnant, which does not mean that you will be menopause. Only the fact of removing the two ovaries will led to the menopause and its demonstrations such as hot flashes and night sweats. You will be able, in this case, to discuss with your doctor the possibility of a hormonal replacement therapy (HRT). If you are postmenopausal before the intervention, there will be no specific modification.
The hysterectomy does not modify the possibility or the quality of sexual intercourses. There is no reason for you to get symptoms such as a gain of weight or a depression, sometimes charged to the hysterectomy. The operational part (the uterus +/- ovaries) is always analyzed and the result of this analysis will be communicated to you in postoperative consultation.
Risks & Complications
In spite of the meticulous surgery technics, it is not possible to guarantee neither therapeutic success nor a total absence of any complications.
During the intervention
- The abdominal opening: the access incision can be modified (“laparoconversion”, i.e. from a laparoscopically assisted hysterectomy to a laparotomy one) according to the observations made during the operation, or if any per-operational complications occurred.
- Significant blood loss: may rarely lead to a blood transfusion.
- Lesions of an organ close to the uterus: this can exceptionally happen: intestinal, urinary tracts or blood vessels wounds, requiring a specific surgical assumption.
Post-operation
- Blood tumor or abscess in the abdominal wall: it generally requires local care, but a surgical evacuation may be an option.
- Lower extremity deep venous thrombosis and pulmonary embolism: in order to prevent this kind of complication, an early rising is recommended, as well as wearing support stockings and daily injections of anticoagulant.
- Bowel obstruction: It can require a medical care, even a surgical operation.
Last update: 10/2/2013